PsychoGenics has been a leader in the field of drug abuse liability for over a decade, specializing in the validation and utilization of rodent models for assessing drug abuse potential.
Our comprehensive range of models and tests, encompassing self-administration, drug discrimination, conditioned place preference, relapse, and withdrawal, delivers critical insights for clients seeking a thorough evaluation of their drug candidates.
The intravenous self-administration (SA) model is widely acknowledged as a highly reliable and predictive method for examining the reinforcing properties of novel therapeutics.
This model serves as a gold standard for drug abuse liability testing, providing valuable insights into the addictive potential of substances and aiding in the development of effective strategies for addiction prevention and treatment.
PsychoGenics applies it to three primary areas:
- Evaluating a compound’s ability to inhibit drug abuse
- Assessing its ability to inhibit reinstatement of drug abuse
- Determining the abuse liability of novel compounds
MTEP inhibits cocaine self-administration
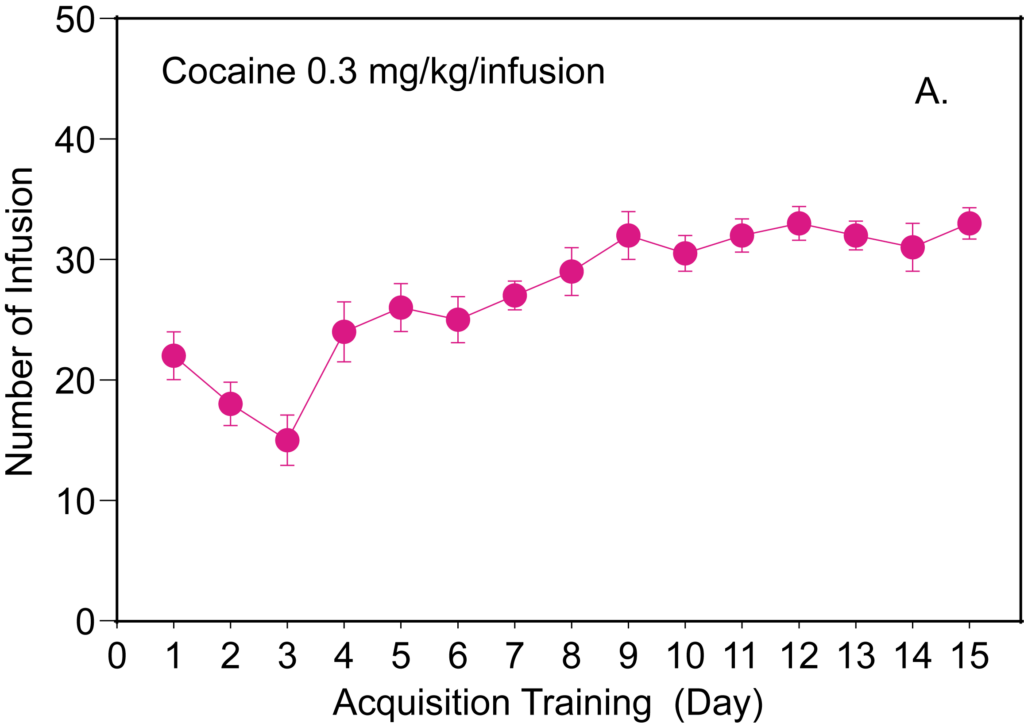

Time course of cocaine self-administration in rats
(3-((2-Methyl-4-thiazolyl)ethynyl) pyridine, a selective allosteric antagonist of mGluR5), decreases cocaine self-administration.
Oxycodone self-administration and its inhibition
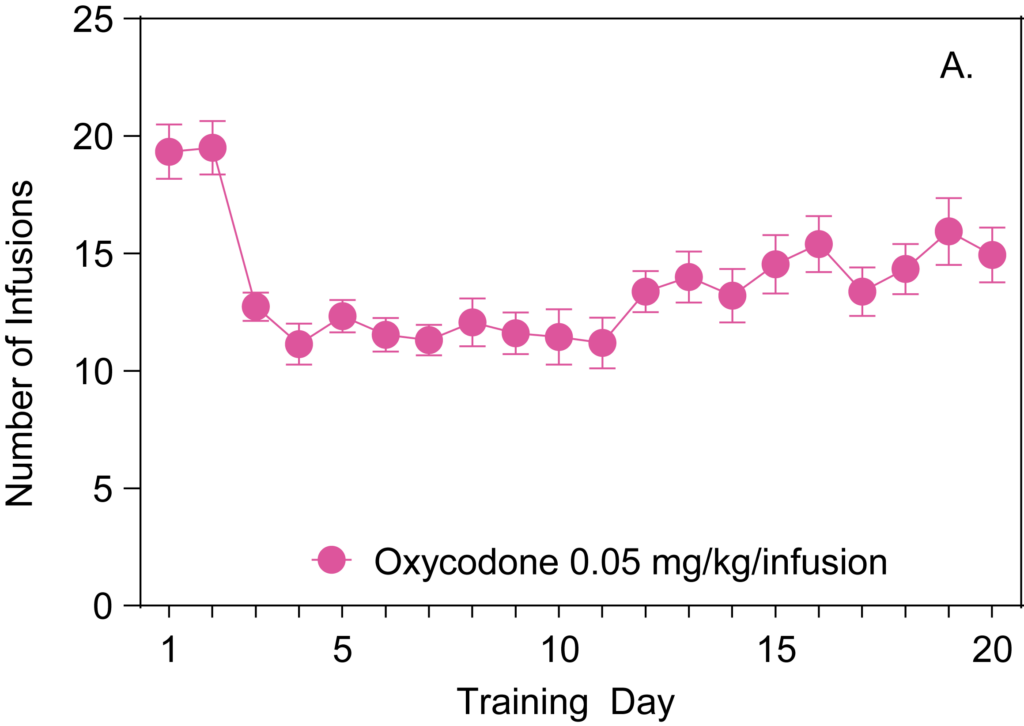
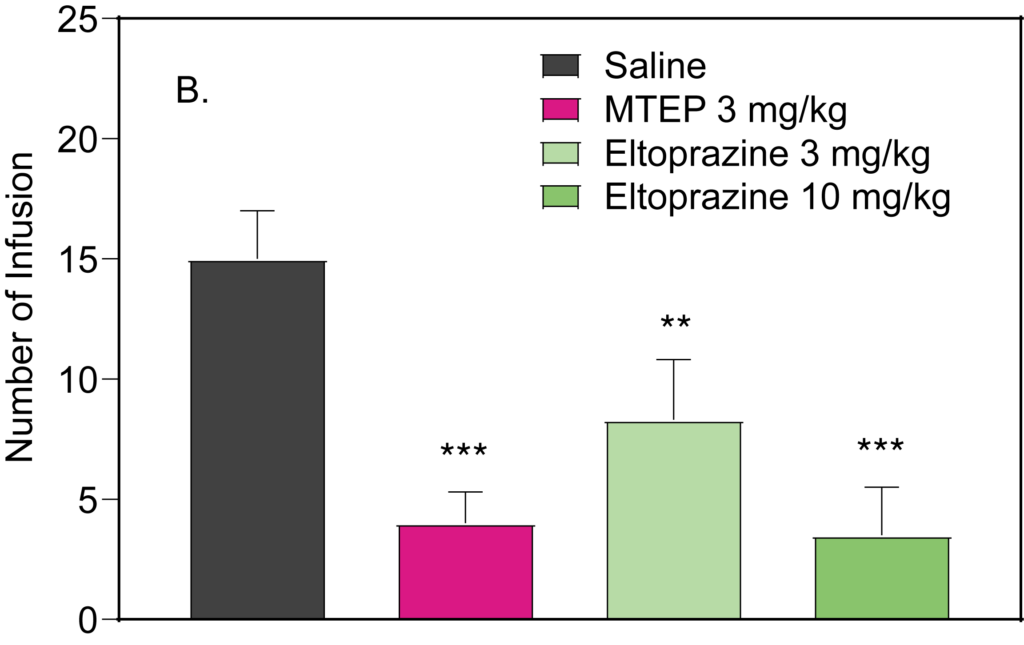
Oxycodone self-administration was acquired through 20 days of training.
MTEP 3 mg/kg and eltoprazine 3 & 10 mg/kg showed efficacy in decreasing oxycodone intake in trained rats.
PR schedule tests with cocaine, morphine and oxycodone
Progressive ratio (PR) schedule is a paradigm used to assess the animal’s motivation to obtain a drug.
Cocaine
Morphine
Oxycodone



The Breakpoint of PR schedule provides an important readout of the animal’s motivation to consume abused drugs. Cocaine, morphine and oxycodone show an increase in breakpoint response.
Reinstatement of drug abuse
Cue-induced reinstatement of nicotine abuse and its inhibition by varenicline
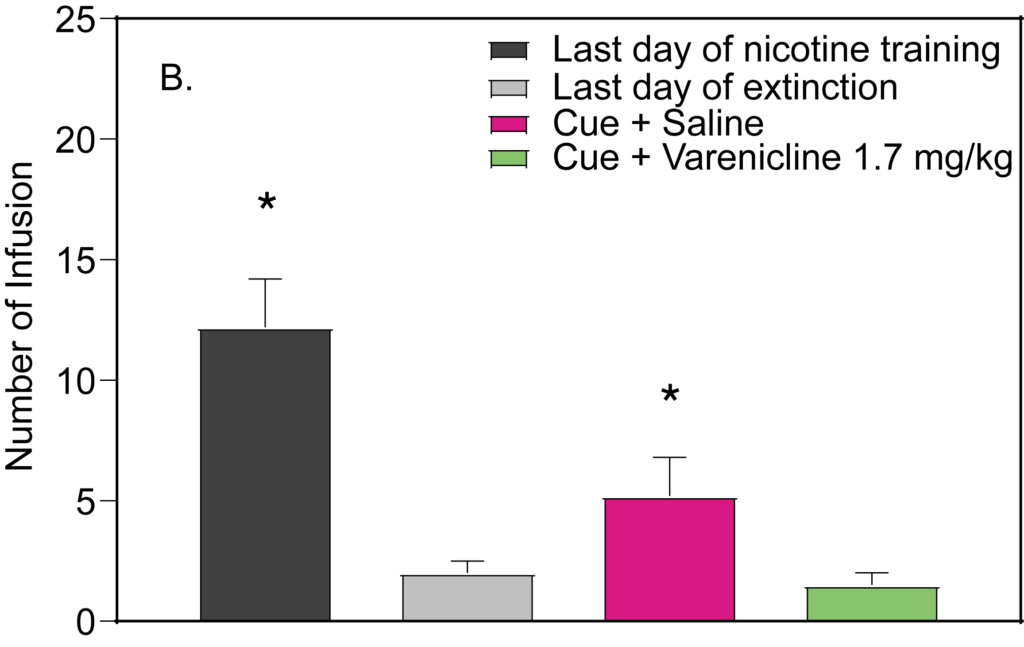
Time course for nicotine self-administration using a cue (tone+light).
Following extinction, exposure to cue only induced reinstatement of nicotine self administration. Varenicline 1.7 mg/kg prevented nicotine reinstatement.
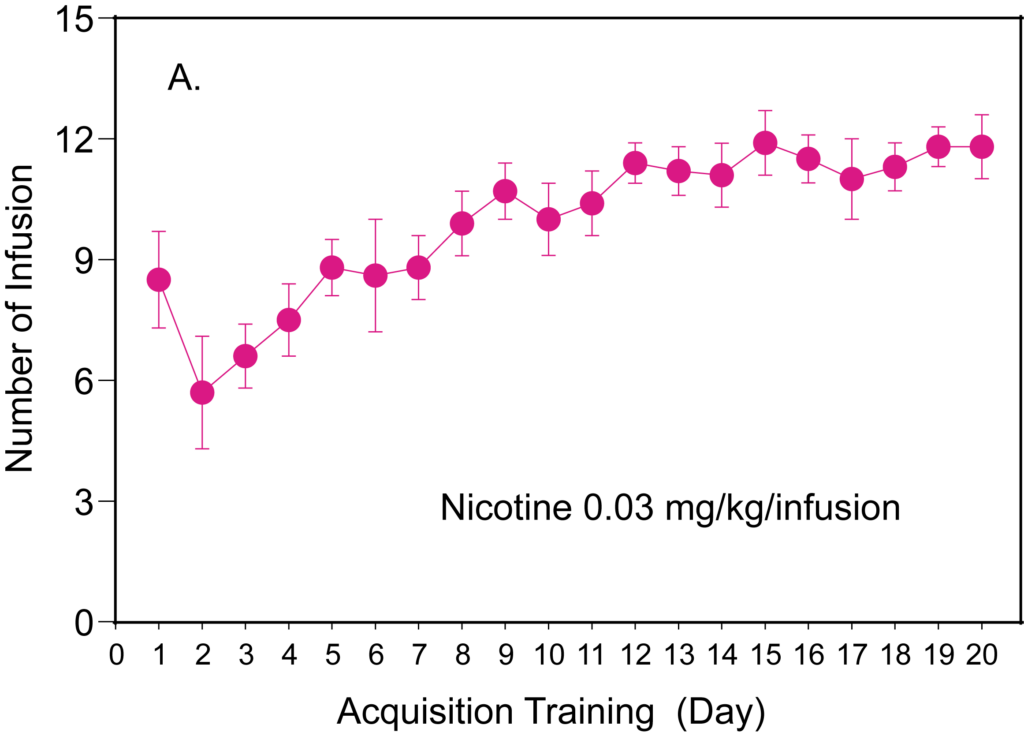
Stress-induced reinstatement of nicotine abuse and its inhibition by eltoprazine
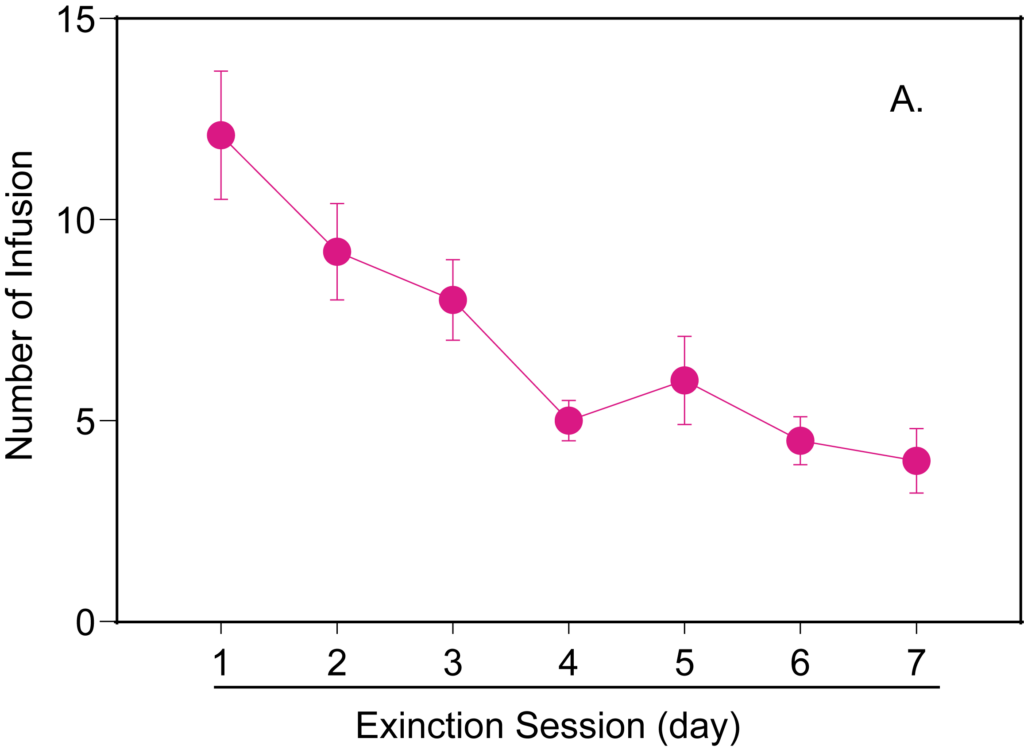
Time course for nicotine (0.03 mg/kg/infusion) extinction session.
Pharmacological stressor yohimbine 2 mg/kg induced significant relapse compared to the last extinction day. Eltoprazine (10 mg/kg) significantly inhibited yohimbine-induced reinstatement.
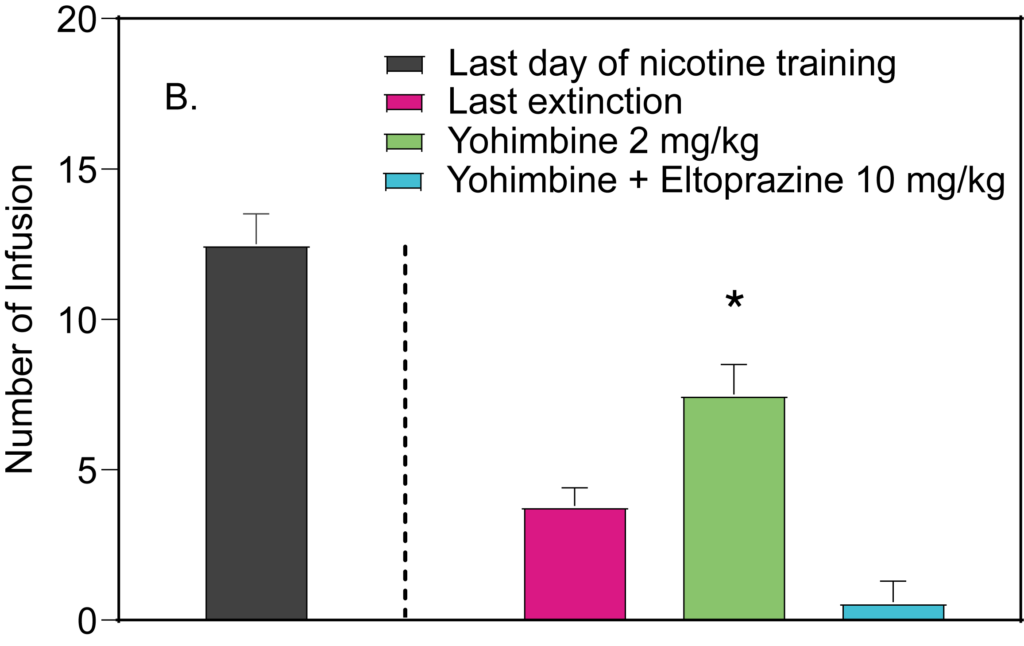
Drug discrimination (DD) is a central behavioral assay that measures the extent to which interoceptive stimulus effects align with those of relevant drugs of abuse. Through DD training, animals are conditioned to exhibit a specific response, such as pressing a particular lever following the administration of a known drug of abuse, and a different response after receiving a placebo or vehicle.
When exposed to a novel compound, the level of drug-appropriate responding indicates the degree of similarity between the subjective effects of the compound and the reference drug.
By combining drug self-administration and drug discrimination models, PsychoGenics provides a crucial source of data for developing medications that maximize therapeutic benefits while minimizing the risk of drug abuse.
Substitution
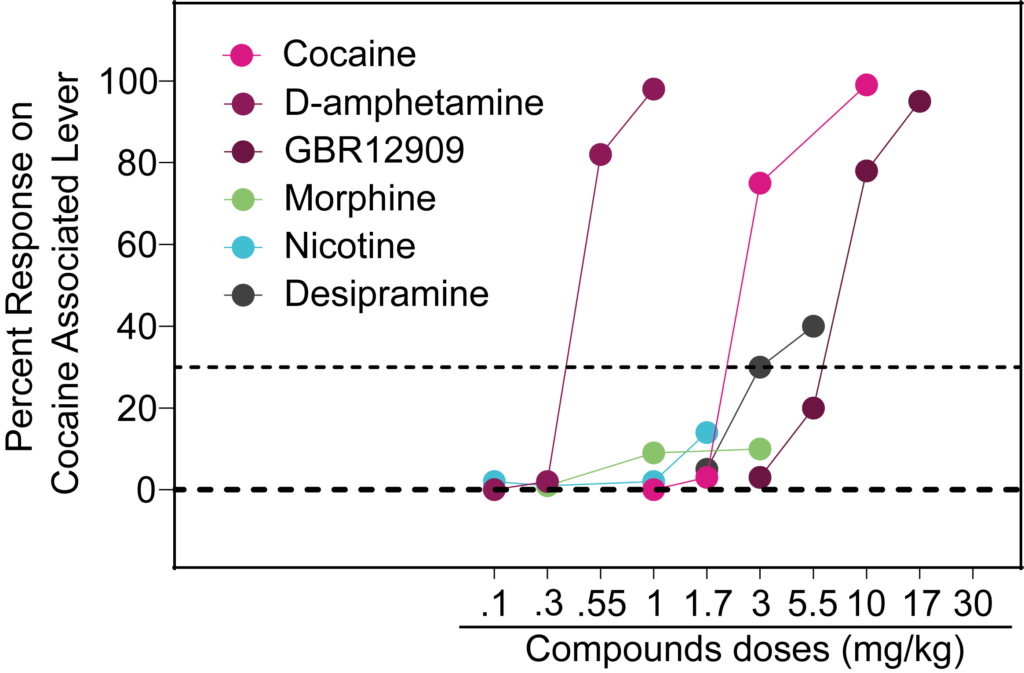
In cocaine-trained rats, d-amphetamine and GBR 12909 (a dopamine reuptake inhibitor) achieved full substitution. Desipramine (a tricyclic antidepressant) showed partial substitution and neither morphine nor nicotine showed substitution.
Rooted in Pavlovian conditioning, conditioned place preference (CPP) is widely utilized to assess preferences for environmental stimuli associated with positive experiences like food, reinforcing drugs, or pain relief linked with distinct cues. CPP detects both reward-driven behaviors and aversion relief, evidenced by animals gravitating toward spaces associated with positive cues.
Morphine and oxycodone-induced CPP
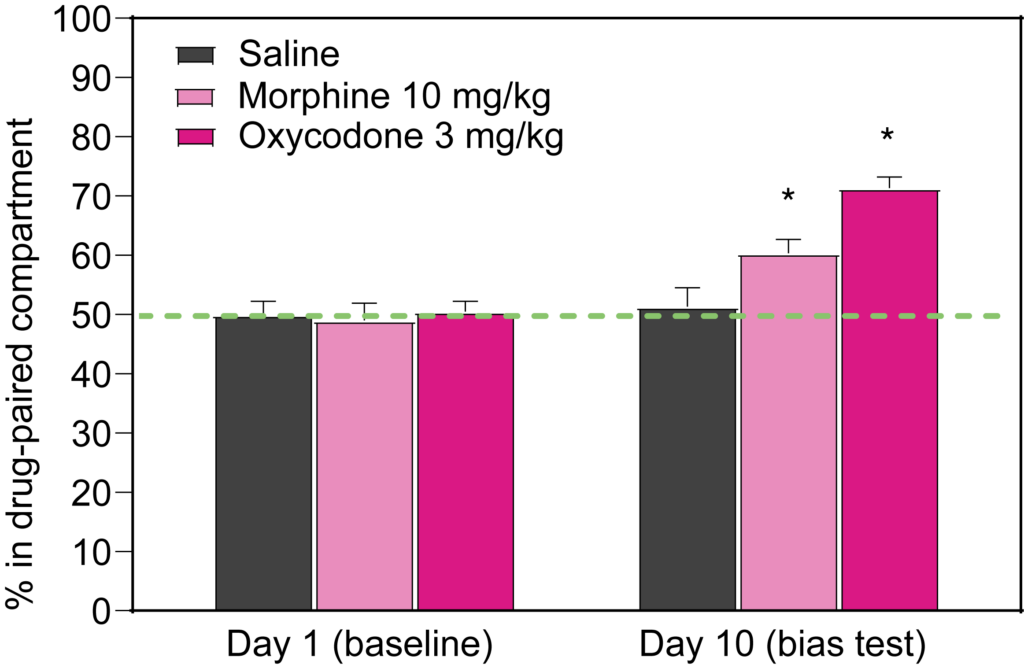

Both morphine (10 mg/kg) and oxycodone (3 mg/kg) induce CPP in rats.
Oxycodone (3 mg/kg) induces CPP in rats. Treatment with MTEP (3 mg/kg) attenuates oxycodone-induced CPP.
In rats, acute withdrawal following chronic administration of a drug may be spontaneous or it can be precipitated with an antagonist. In rats, withdrawal from a drug of abuse can human withdrawal syndrome, including somatic signs like tremors, abdominal constrictions, tremor, diarrhea, ptosis, headshakes, irritability and mimic other symptoms.
Nicotine: Precipitated Withdrawal
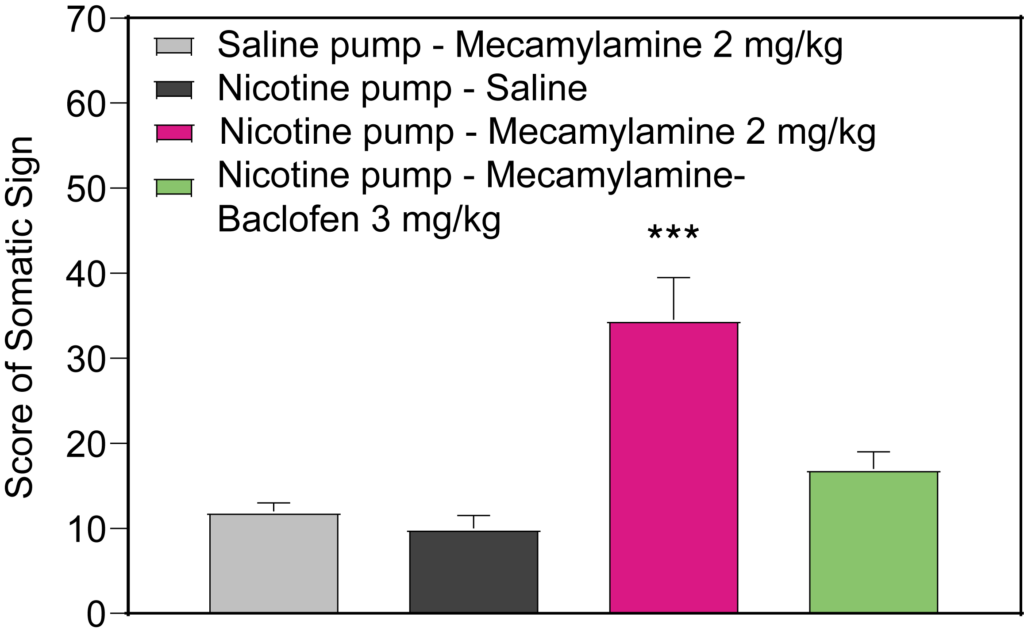
Rats were administered nicotine (18mg/kg/day) via a subcutaneous osmotic pump for 14 days. Mecamylamine (2 mg/kg) induced precipitated withdrawal as measured by the increased number of withdrawal symptoms. Treatment with baclofen (3 mg/kg) attenuated mecamylamine-induced withdrawal symptoms.
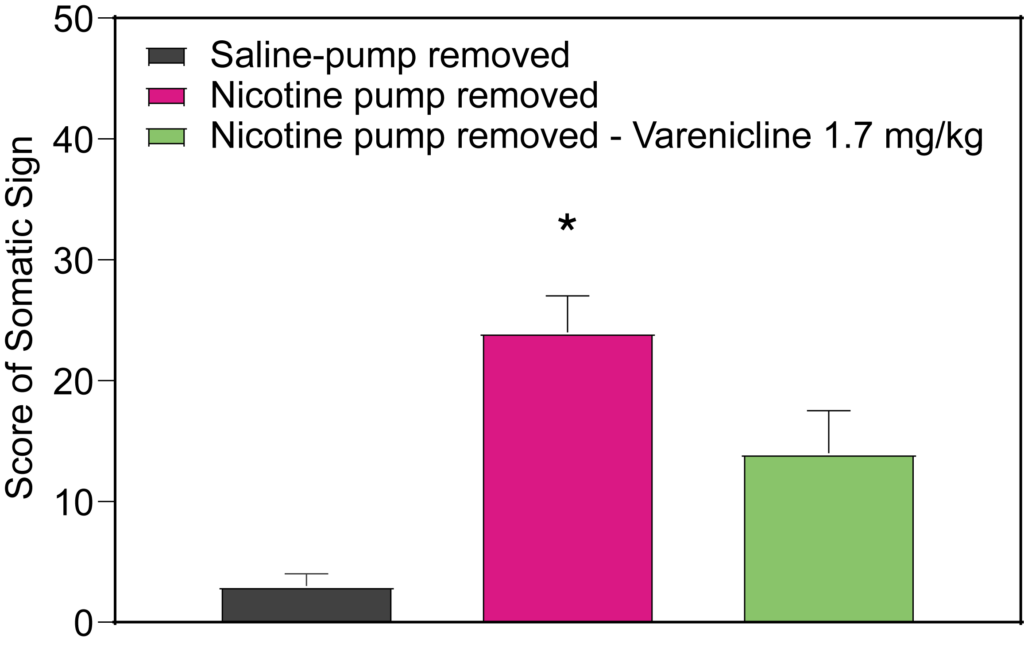
Rats were administered nicotine (18mg/kg/day) via a subcutaneous osmotic pump for 21 days after which the pump was removed. Rats showed spontaneous withdrawal symptoms 24 hours after cessation of nicotine administration. Varenicline (1.7 mg/kg) attenuated spontaneous withdrawal symptoms.